Why Reproductive Health Matters More Than Ever
Imagine walking through any Indian city today and observing the massive billboards advertising family planning services, the increasing awareness campaigns about sexually transmitted diseases, or the growing number of fertility clinics offering advanced reproductive technologies. What you’re witnessing is the real-world application of reproductive health – a field that has become crucial not just for individual well-being, but for the sustainable development of our entire society.
Every day, millions of couples worldwide make decisions about family planning, thousands of healthcare workers counsel patients about contraceptive methods, and countless researchers work tirelessly to develop better reproductive technologies. From the teenage student learning about safe practices to the married couple planning their family size, reproductive health touches every aspect of human society.
This chapter isn’t just about memorizing definitions for your CBSE exam – it’s about understanding the biological foundations that govern one of the most fundamental aspects of human existence. When you study reproductive health, you’re exploring how scientific advances have revolutionized human fertility control, disease prevention, and assisted reproduction. You’re learning about technologies that have transformed the lives of millions, from the development of the contraceptive pill in the 1960s to the birth of the first IVF baby in 1978.
As a CBSE Class 12 Biology student, you’re not just preparing for an examination; you’re building the foundation for understanding one of the most rapidly evolving fields in modern medicine and biotechnology. The concepts you’ll master here connect directly to career paths in medicine, biotechnology, public health, and biomedical research.
Learning Objectives
By the end of this comprehensive study guide, you will be able to:
- Analyze the fundamental need for reproductive health and explain its significance in personal and societal contexts
- Evaluate different contraceptive methods and recommend appropriate choices based on biological mechanisms and effectiveness
- Identify and explain prevention strategies for sexually transmitted diseases with detailed biological understanding
- Understand the medical and ethical aspects of Medical Termination of Pregnancy (MTP) procedures
- Explain the scientific basis and applications of amniocentesis in genetic screening
- Compare and contrast assisted reproductive technologies including IVF, ZIFT, and GIFT procedures
- Apply reproductive health concepts to solve complex biological problems and case studies
- Connect reproductive health principles to current biotechnology developments and medical practices
1: Understanding Reproductive Health – Foundation and Significance
What Makes Reproductive Health Essential?
Reproductive health isn’t just about preventing pregnancy or treating infertility – it’s a comprehensive approach to ensuring complete physical, mental, and social well-being in all matters related to the reproductive system. Think of it as the biological equivalent of maintaining a sophisticated machinery where every component must function optimally for the entire system to work effectively.
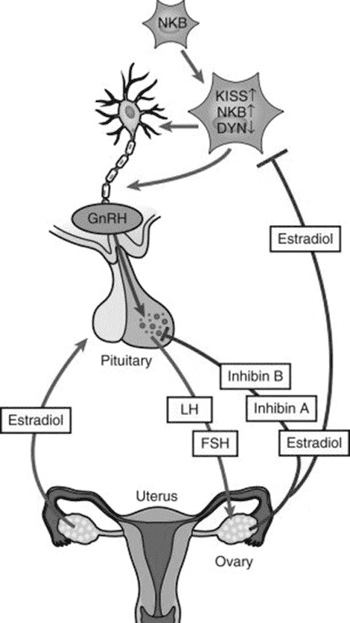
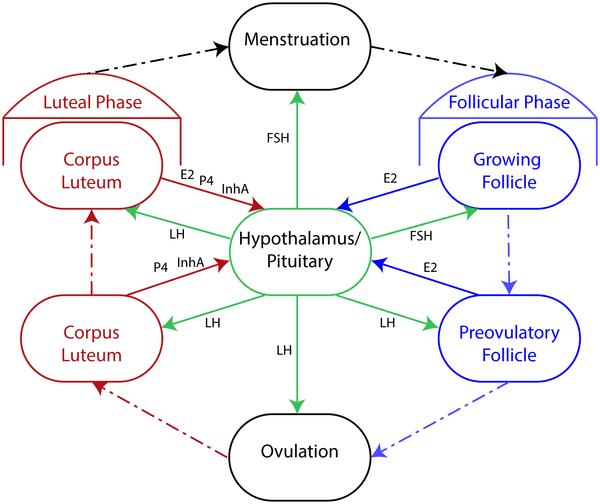
When we examine reproductive health from a biological perspective, we’re looking at the intricate interplay between hormonal regulation, anatomical structures, physiological processes, and environmental factors. Consider how the human reproductive system operates like a precisely timed orchestra – the hypothalamus releases GnRH, the pituitary responds with FSH and LH, the gonads produce sex hormones, and the reproductive organs undergo cyclical changes. Any disruption in this delicate balance can lead to reproductive health issues.
The Biological Foundation of Reproductive Health
Your reproductive system doesn’t operate in isolation – it’s intimately connected with your endocrine system, immune system, and overall health status. For instance, stress hormones like cortisol can suppress reproductive hormone production, explaining why chronic stress often leads to fertility problems. Similarly, nutritional deficiencies can affect gamete production and hormone synthesis, highlighting the interconnected nature of biological systems.
Understanding reproductive health requires appreciating both the microscopic cellular processes and the macroscopic physiological functions. At the cellular level, reproductive health involves proper DNA replication during gametogenesis, optimal hormone receptor function, and effective cellular communication. At the organ level, it encompasses proper functioning of reproductive organs, efficient hormone production, and coordinated physiological responses.
Real-World Biology Connection: The global fertility rate has declined from 5.0 children per woman in 1960 to approximately 2.4 in 2020, largely due to improved reproductive health education and access to family planning services. This demographic transition demonstrates how biological knowledge translates into societal changes.
Population Dynamics and Reproductive Health
From an ecological perspective, human reproductive health directly impacts population dynamics and resource sustainability. When you study population growth curves in ecology, you’re seeing the real-world applications of reproductive health policies. Countries with comprehensive reproductive health programs often achieve demographic transitions more smoothly, balancing population growth with resource availability.
The biological principle of carrying capacity applies to human populations just as it does to other species. Reproductive health education and services help populations approach their carrying capacity gradually rather than experiencing the boom-and-bust cycles seen in some animal populations. This biological understanding underlies many governmental policies on family planning and reproductive health.
2: The Science of Contraception – Biological Mechanisms and Methods
Understanding Contraceptive Mechanisms at the Cellular Level
Contraception works by interfering with the normal reproductive process at various biological levels. To truly understand contraceptive methods, you need to appreciate where and how each method interrupts the pathway from gamete production to embryo implantation.
The human reproductive process involves several critical steps: gametogenesis, ovulation, fertilization, early embryonic development, and implantation. Contraceptive methods target specific steps in this sequence, and understanding these intervention points helps you appreciate why different methods have varying effectiveness rates and side effects.
Let’s examine this process systematically:
- Gametogenesis Phase: Sperm production takes approximately 74 days, while oocytes complete meiosis I during ovulation. Some contraceptive methods, like hormonal contraceptives, affect this phase by suppressing FSH and LH production.
- Ovulation Phase: The LH surge triggers ovulation around day 14 of a 28-day cycle. Hormonal contraceptives prevent this surge, effectively blocking ovulation.
- Fertilization Phase: Sperm must travel through the female reproductive tract and penetrate the egg. Barrier methods and spermicides interfere with this phase.
- Implantation Phase: The blastocyst must successfully implant in the endometrium. Some contraceptives alter the endometrial lining, making implantation less likely.
Natural Methods: Understanding Biological Rhythms
Natural family planning methods rely on understanding the precise biological timing of the female reproductive cycle. These methods require detailed knowledge of hormonal fluctuations, physiological changes, and fertility indicators.
Rhythm Method (Calendar Method): This method is based on the biological fact that human eggs remain viable for only 12-24 hours after ovulation, while sperm can survive in the female reproductive tract for up to 5 days. By identifying the fertile period, couples can avoid intercourse during this time.
The biological basis involves tracking the menstrual cycle pattern over several months to predict ovulation timing. However, this method has limitations because ovulation timing can vary due to stress, illness, or hormonal fluctuations. The failure rate is relatively high (20-30%) because it doesn’t account for cycle irregularities.
Basal Body Temperature Method: This method exploits the biological fact that progesterone, produced after ovulation, causes a slight increase (0.2-0.5°C) in basal body temperature. By monitoring temperature daily, women can identify when ovulation has occurred.
The biological mechanism involves progesterone’s thermogenic effect on the hypothalamus. After ovulation, the corpus luteum produces progesterone, which acts on the temperature-regulating center in the brain. This method is more reliable than the calendar method but requires consistent daily monitoring.
Cervical Mucus Method: The cervix produces different types of mucus throughout the menstrual cycle, influenced by estrogen and progesterone levels. Around ovulation, high estrogen levels cause the production of clear, stretchy mucus that facilitates sperm transport.
Barrier Methods: Physical and Chemical Barriers
Barrier methods work by preventing sperm from reaching the egg through physical or chemical means. Understanding their biological effectiveness requires examining how they interact with reproductive physiology.
Condoms: Male and female condoms create a physical barrier that prevents sperm from entering the female reproductive tract. The biological effectiveness depends on proper usage and the integrity of the barrier material. Latex condoms also provide protection against sexually transmitted infections by preventing the exchange of bodily fluids.
From a biological perspective, condoms are highly effective (98% when used correctly) because they completely block sperm transport. However, real-world effectiveness is lower (85%) due to user errors like improper application or breakage.
Diaphragms and Cervical Caps: These methods create a barrier at the cervix, preventing sperm from entering the uterus. They’re often used with spermicidal agents to increase effectiveness. The biological principle involves blocking the internal os of the cervix, which is the natural pathway for sperm ascent.
Spermicides: These chemicals, typically containing nonoxynol-9, work by disrupting sperm cell membranes and reducing sperm motility. The biological mechanism involves the surfactant properties of these chemicals, which break down the lipid bilayer of sperm cell membranes, causing cell death.
Hormonal Methods: Manipulating Endocrine Pathways
Hormonal contraceptives represent one of the most sophisticated applications of endocrine biology in medicine. These methods work by mimicking or altering natural hormone patterns to prevent pregnancy.
Combined Oral Contraceptives (Birth Control Pills): These contain synthetic versions of estrogen and progesterone that suppress the hypothalamic-pituitary-ovarian axis through negative feedback mechanisms.
The biological mechanism involves several pathways:
- Hypothalamic Suppression: Synthetic hormones suppress GnRH release from the hypothalamus through negative feedback, similar to the natural luteal phase of the menstrual cycle.
- Pituitary Suppression: Reduced GnRH leads to suppressed FSH and LH production, preventing follicular development and ovulation.
- Endometrial Changes: Synthetic progestins alter the endometrial lining, making it less suitable for implantation.
- Cervical Mucus Changes: Progestins increase cervical mucus viscosity, creating a barrier to sperm penetration.
Progestin-Only Pills (Mini-Pills): These work primarily by altering cervical mucus and endometrial lining rather than completely suppressing ovulation. The biological advantage is fewer side effects related to estrogen, but they require more precise timing for effectiveness.
Long-Acting Hormonal Methods: Injectable contraceptives (Depo-Provera), implants (Norplant), and hormonal IUDs provide extended pregnancy prevention through sustained hormone release. The biological advantage is consistent hormone levels without daily user intervention.
Intrauterine Devices (IUDs): Local and Systemic Effects
IUDs work through multiple biological mechanisms that create an inhospitable environment for fertilization and implantation.
Copper IUDs: Copper ions released from the device create a toxic environment for sperm and eggs. The biological mechanism involves copper’s antimicrobial properties and its ability to generate reactive oxygen species that damage sperm membranes and reduce sperm motility.
Hormonal IUDs: These release progestins directly into the uterine cavity, causing local effects on the endometrium and cervical mucus while minimizing systemic hormone exposure.
Surgical Methods: Permanent Sterilization
Surgical contraception involves blocking or removing parts of the reproductive tract to prevent gamete transport permanently.
Vasectomy: This procedure involves cutting or blocking the vas deferens to prevent sperm from mixing with seminal fluid. The biological principle relies on the fact that sperm constitute only 2-3% of semen volume, so their absence doesn’t significantly affect ejaculate volume but completely prevents fertilization.
Tubal Ligation: This procedure blocks the fallopian tubes, preventing eggs from traveling to the uterus and sperm from reaching the eggs. Various techniques exist, including cutting, sealing, or blocking the tubes.
Biology Check: Can you explain why hormonal contraceptives are nearly 100% effective when used perfectly, but only 92% effective in typical use? Consider the biological requirements for these methods to work effectively.
3: Sexually Transmitted Diseases – Understanding Pathogenesis and Prevention
The Biological Basis of STD Transmission
Sexually transmitted diseases represent a fascinating intersection of microbiology, immunology, and reproductive biology. Understanding STDs requires appreciating how pathogens exploit the intimate contact involved in sexual reproduction to ensure their own transmission and survival.
From an evolutionary perspective, sexually transmitted pathogens have developed sophisticated mechanisms to persist in host populations. They often cause chronic infections with periods of high infectivity coinciding with sexual activity, ensuring efficient transmission to new hosts. This biological strategy explains why many STDs remain prevalent despite medical advances.
Pathogen Types and Transmission Mechanisms
STDs are caused by various types of microorganisms, each with unique biological characteristics that influence their transmission patterns and health effects.
Bacterial STDs: Organisms like Neisseria gonorrhoeae, Chlamydia trachomatis, and Treponema pallidum cause gonorrhea, chlamydia, and syphilis respectively. These bacteria have evolved specific adhesion mechanisms that allow them to colonize the urogenital tract’s mucous membranes.
The biological advantage of sexual transmission for these bacteria lies in the direct transfer between hosts without exposure to harsh environmental conditions. The warm, moist environment of the reproductive tract provides optimal conditions for bacterial survival and multiplication.
Viral STDs: Human Papillomavirus (HPV), Herpes Simplex Virus (HSV), and Human Immunodeficiency Virus (HIV) represent major viral STDs. These viruses have developed mechanisms to establish persistent infections, often integrating into host cell DNA or remaining dormant in nerve cells.
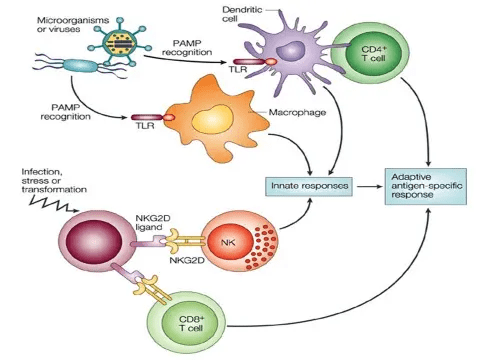
HIV provides an excellent example of how STD pathogens exploit human biology. The virus specifically targets CD4+ T helper cells, which are crucial for coordinating immune responses. By destroying these cells, HIV gradually compromises the immune system, making patients susceptible to opportunistic infections.
The biological mechanism involves:
- Viral Attachment: HIV binds to CD4 receptors and coreceptors (CCR5 or CXCR4) on T helper cells
- Membrane Fusion: The viral envelope fuses with the host cell membrane
- Reverse Transcription: Viral RNA is converted to DNA using reverse transcriptase
- Integration: Viral DNA integrates into the host cell chromosome
- Viral Replication: New virus particles are produced and released
- Cell Death: Infected cells eventually die, reducing immune function
Parasitic STDs: Trichomonas vaginalis causes trichomoniasis, demonstrating how parasitic organisms can exploit sexual transmission. This protozoan has adapted to survive in the urogenital tract’s specific pH and oxygen conditions.
Understanding Disease Progression and Symptoms
The biological progression of STDs often follows predictable patterns based on the pathogen type and host immune responses. Understanding these patterns helps in early detection and appropriate treatment.
Primary Infection Phase: Most STDs begin with an initial infection at the site of pathogen entry. During this phase, local immune responses may cause inflammation, leading to symptoms like discharge, burning, or lesions.
Systemic Spread Phase: Many STDs can spread beyond the initial infection site. For example, untreated gonorrhea can ascend from the cervix to cause pelvic inflammatory disease (PID), potentially affecting the fallopian tubes and ovaries.
Chronic/Latent Phase: Some STDs establish chronic infections with periods of active disease alternating with asymptomatic phases. HSV exemplifies this pattern, with initial outbreaks followed by viral dormancy in nerve ganglia and periodic reactivations.
Prevention Strategies: Biological and Behavioral Approaches
Effective STD prevention requires understanding both the biological vulnerabilities of pathogens and the behavioral factors that influence transmission.
Barrier Protection: Condoms represent the most effective biological barrier against STD transmission. Their effectiveness varies by pathogen type:
- Nearly 100% effective against HIV and gonorrhea (transmitted through genital fluids)
- Less effective against HSV and HPV (transmitted through skin contact)
The biological principle involves preventing contact between infected tissues/fluids and susceptible mucous membranes. However, effectiveness depends on consistent and correct usage.
Vaccination: Several vaccines target STD pathogens by stimulating adaptive immune responses:
HPV Vaccination: The HPV vaccine contains virus-like particles that stimulate antibody production without causing infection. This biological approach has dramatically reduced HPV infections in vaccinated populations.
Hepatitis B Vaccination: This vaccine protects against hepatitis B virus, which can be sexually transmitted. The biological mechanism involves presenting viral surface antigens to the immune system, promoting memory cell formation.
Screening and Early Detection: Regular screening exploits the biological fact that early-stage STDs are often more treatable than advanced infections. Screening programs target high-risk populations and use sensitive detection methods like PCR amplification.
Partner Treatment: The biological rationale for treating sexual partners simultaneously stems from the high likelihood of mutual infection. Without partner treatment, reinfection commonly occurs, maintaining the pathogen in the population.
Antimicrobial Resistance: An Evolving Challenge
The development of antimicrobial resistance in STD pathogens represents natural selection in action. Understanding this biological process helps explain why combination therapies and careful antibiotic use are essential.
Resistance Mechanisms: Bacteria develop resistance through various biological mechanisms:
- Enzymatic Degradation: Producing enzymes that break down antibiotics
- Target Modification: Altering the antibiotic’s target protein
- Efflux Pumps: Actively removing antibiotics from bacterial cells
- Reduced Permeability: Preventing antibiotic entry into bacterial cells
Real-World Biology Connection: Gonorrhea has developed resistance to multiple antibiotics over the decades, with some strains now showing reduced susceptibility to the last-line treatment options. This evolution demonstrates natural selection pressure created by antibiotic use.
4: Medical Termination of Pregnancy – Biological Processes and Ethical Considerations
Understanding Early Pregnancy Biology
To comprehend Medical Termination of Pregnancy (MTP), you must first understand the biological processes of early pregnancy development and the physiological changes that occur during the first trimester.
Embryonic Development Timeline: Human embryonic development follows a precise biological schedule:
- Week 1-2: Fertilization, cleavage, and blastocyst formation
- Week 3: Gastrulation and neural tube formation
- Week 4-8: Organogenesis and major organ system development
- Week 9-12: Continued organ development and growth
Hormonal Changes in Early Pregnancy: Successful pregnancy requires complex hormonal coordination:
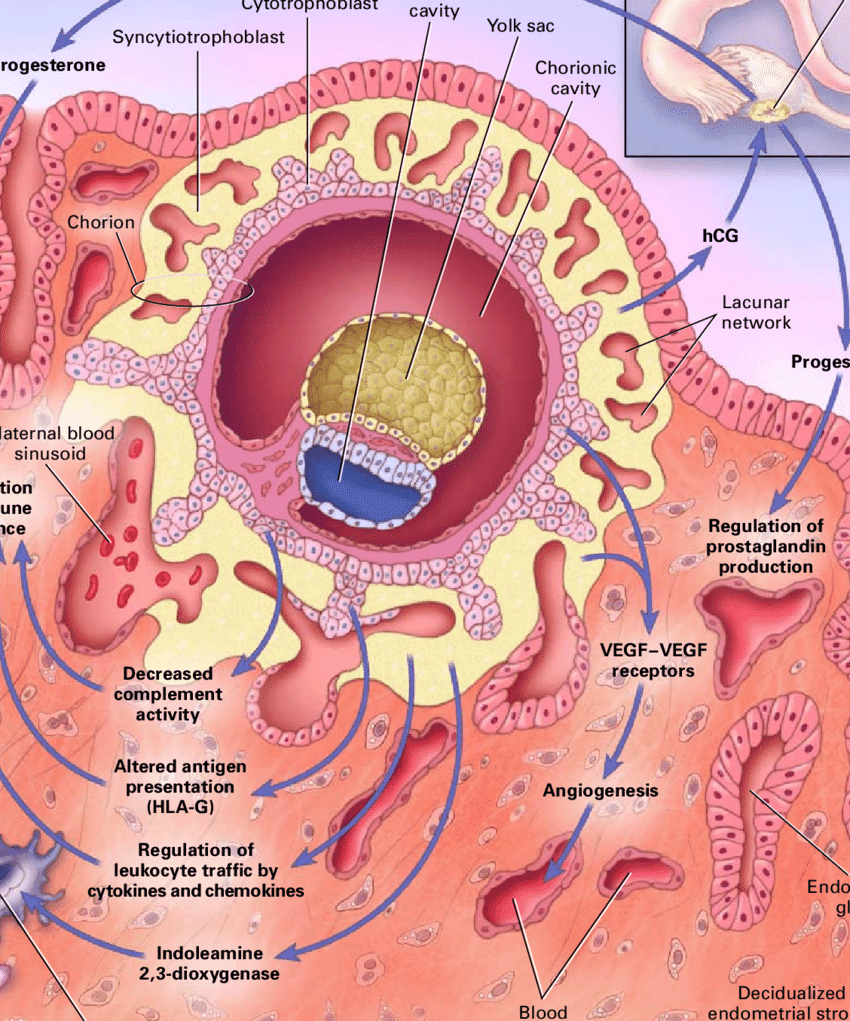
PROCESS: Hormonal Maintenance of Early Pregnancy
- hCG Production: The developing embryo produces human chorionic gonadotropin (hCG), which maintains the corpus luteum
- Progesterone Maintenance: The corpus luteum continues producing progesterone, preventing menstruation
- Endometrial Support: Progesterone maintains the thickened endometrium necessary for embryo support
- Estrogen Production: Increasing estrogen levels support continued pregnancy maintenance
Understanding these biological processes helps explain how MTP procedures work and why timing is crucial for safety and effectiveness.
Methods of Medical Termination
MTP can be accomplished through medical (pharmaceutical) or surgical methods, each exploiting different biological mechanisms.
Medical Abortion Using Medications:
Mifepristone (RU-486): This synthetic steroid works as a progesterone receptor antagonist. The biological mechanism involves:
- Receptor Blocking: Mifepristone binds to progesterone receptors but doesn’t activate them
- Decidual Breakdown: Without progesterone signaling, the endometrium begins to shed
- Cervical Softening: Loss of progesterone effects causes cervical softening and dilation
Misoprostol: This prostaglandin E1 analog induces uterine contractions through:
- Smooth Muscle Stimulation: Prostaglandins bind to specific receptors on uterine smooth muscle
- Calcium Release: This binding triggers intracellular calcium release
- Muscle Contraction: Increased calcium causes sustained uterine contractions
- Cervical Dilation: Prostaglandins also promote cervical ripening and dilation
The combination of mifepristone followed by misoprostol is highly effective (95-98%) for early pregnancy termination because it addresses both hormonal maintenance and physical expulsion.
Surgical Methods:
Vacuum Aspiration: This procedure physically removes pregnancy tissue through suction. The biological rationale involves disrupting the embryo-endometrial connection and removing pregnancy products before they can re-establish.
Dilation and Curettage (D&C): This method involves dilating the cervix and scraping the uterine lining. While effective, it carries higher risks of complications compared to vacuum aspiration.
Safety Considerations and Biological Risks
The safety of MTP procedures depends on several biological factors:
Gestational Age: Earlier procedures are generally safer because:
- The embryo/fetus is smaller and easier to remove completely
- Hormonal changes are less established
- Uterine size and vascularity are closer to non-pregnant state
- Risk of complications increases with gestational age
Incomplete Abortion: This complication occurs when pregnancy tissue remains in the uterus, potentially leading to:
- Continued pregnancy hormone production
- Infection risk due to retained tissue
- Bleeding complications
- Need for additional procedures
Infection Risk: The biological basis for infection risk involves:
- Disrupted endometrial barrier function
- Potential introduction of bacteria during procedures
- Compromised local immune responses
- Importance of sterile technique and prophylactic antibiotics
Legal and Ethical Framework in India
India’s Medical Termination of Pregnancy Act provides a legal framework that balances reproductive rights with ethical considerations:
Legal Indications: The act allows MTP when:
- Continuation of pregnancy risks the woman’s life
- Pregnancy results from rape or contraceptive failure
- Substantial risk exists of serious fetal abnormalities
Gestational Age Limits: Different rules apply based on biological development:
- Up to 20 weeks: Single doctor’s opinion sufficient for specified indications
- Beyond 20 weeks: Requires medical board approval for severe fetal abnormalities
Healthcare Provider Requirements: Only registered medical practitioners can perform MTP procedures, ensuring appropriate medical training and facility standards.
Biology Check: Why is the combination of mifepristone followed by misoprostol more effective than either drug alone? Consider the different biological pathways each drug affects.
5: Amniocentesis – Genetic Screening and Prenatal Diagnosis
The Biological Foundation of Prenatal Genetic Testing
Amniocentesis represents one of the most sophisticated applications of developmental biology and genetics in clinical medicine. This procedure exploits the biological fact that amniotic fluid contains fetal cells that carry the complete genetic information of the developing fetus.
Embryological Basis of Amniotic Fluid Formation:
During early embryonic development, the amniotic cavity forms around the developing embryo. The amniotic fluid serves multiple biological functions:
- Physical Protection: Cushioning the fetus from mechanical trauma
- Temperature Regulation: Maintaining stable thermal environment
- Lung Development: Providing fluid for fetal breathing movements
- Musculoskeletal Development: Allowing fetal movement and preventing limb contractures
Cellular Content of Amniotic Fluid:
The amniotic fluid contains various cell types that provide diagnostic information:
- Fetal Skin Cells: Shed from the developing epidermis
- Kidney Cells: Present in fetal urine that mixes with amniotic fluid
- Respiratory Tract Cells: From developing lung tissue
- Gastrointestinal Cells: From the fetal digestive system
These cells are genetically identical to the fetus and can be cultured for chromosomal analysis, making amniocentesis a powerful diagnostic tool.
Timing and Biological Rationale
Optimal Timing: Amniocentesis is typically performed between 15-20 weeks of gestation, based on several biological considerations:
Sufficient Amniotic Fluid Volume: By 15 weeks, approximately 200ml of amniotic fluid is present, allowing safe removal of 15-20ml without significantly reducing fetal protection.
Adequate Cell Concentration: The concentration of viable fetal cells in amniotic fluid reaches diagnostic levels by this gestational age.
Organ Development Status: Most major organ systems have formed by this time, allowing detection of structural abnormalities through associated biochemical markers.
Safe Gestational Window: This timing balances early detection with procedure safety and allows time for decision-making if abnormalities are detected.
Diagnostic Applications and Genetic Analysis
Chromosomal Analysis:
PROCESS: Karyotype Analysis from Amniotic Fluid Cells
- Cell Isolation: Fetal cells are separated from amniotic fluid through centrifugation
- Cell Culture: Cells are grown in culture medium to increase their number
- Metaphase Arrest: Dividing cells are stopped in metaphase using colchicine
- Chromosome Preparation: Cells are treated to spread chromosomes on slides
- Staining and Analysis: Chromosomes are stained and examined for numerical and structural abnormalities
This analysis can detect:
- Down Syndrome (Trisomy 21): Extra chromosome 21
- Edwards Syndrome (Trisomy 18): Extra chromosome 18
- Patau Syndrome (Trisomy 13): Extra chromosome 13
- Sex Chromosome Abnormalities: Turner syndrome, Klinefelter syndrome
- Structural Chromosomal Rearrangements: Deletions, duplications, translocations
Molecular Genetic Testing:
Modern amniocentesis can also detect single-gene disorders through DNA analysis:
- Cystic Fibrosis: Mutations in the CFTR gene
- Sickle Cell Disease: Mutations in the beta-globin gene
- Huntington’s Disease: CAG repeat expansions in the HTT gene
- Duchenne Muscular Dystrophy: Deletions in the dystrophin gene
Biochemical Analysis:
Amniotic fluid contains various biomolecules that can indicate fetal abnormalities:
- Alpha-fetoprotein (AFP): Elevated levels may indicate neural tube defects
- Acetylcholinesterase: Present in cases of open neural tube defects
- Lecithin/Sphingomyelin Ratio: Indicates fetal lung maturity
Procedure Safety and Biological Risks
Procedure Technique: Amniocentesis involves inserting a thin needle through the maternal abdomen into the amniotic sac under ultrasound guidance. The biological safety depends on several factors:
Placental Localization: Ultrasound guidance ensures the needle avoids the placenta, preventing potential bleeding complications and reducing infection risk.
Fetal Position: The procedure is performed when the fetus is positioned to minimize contact with the needle.
Sterile Technique: Proper sterilization prevents introduction of maternal bacteria into the amniotic environment.
Risk Assessment: The biological risks include:
Miscarriage Risk: Approximately 1 in 300-500 procedures may result in pregnancy loss, though recent studies suggest the risk may be lower with experienced practitioners.
Infection: Rare but serious risk if bacteria are introduced into the amniotic cavity.
Maternal Injury: Extremely rare risk of injury to maternal organs.
Maternal-Fetal Bleeding: Small risk of mixing maternal and fetal blood, which can be significant if the mother is Rh-negative and the fetus is Rh-positive.
Ethical Considerations and Decision-Making
Informed Consent Process: The biological complexity of genetic conditions requires comprehensive counseling about:
- Accuracy and limitations of testing
- Potential for inconclusive results
- Implications of positive findings
- Available management options
Sex Selection Concerns: In India, amniocentesis for sex determination is prohibited by law due to concerns about female feticide. The biological ability to determine fetal sex creates ethical challenges that require careful regulation.
Genetic Counseling: Understanding genetic test results requires expertise in:
- Inheritance patterns and recurrence risks
- Phenotypic variability of genetic conditions
- Available treatments and management options
- Psychosocial implications for families
Real-World Biology Connection: The development of non-invasive prenatal testing (NIPT) using cell-free fetal DNA in maternal blood represents an evolution in prenatal screening, offering similar information with reduced procedural risk.
6: Assisted Reproductive Technologies – IVF, ZIFT, and GIFT
Understanding Infertility: Biological Causes and Mechanisms
Before exploring assisted reproductive technologies, you must understand the complex biological factors that can impair natural fertility. Infertility affects approximately 10-15% of couples globally, with causes roughly equally distributed between male and female factors.
Male Factor Infertility:
The biological basis of male infertility often involves disruptions in spermatogenesis, sperm transport, or sperm function:
Spermatogenesis Disorders: The process of sperm production takes approximately 74 days and involves complex hormonal regulation. Disruptions can occur due to:
- Hormonal Imbalances: FSH and LH deficiencies affecting Sertoli and Leydig cell function
- Genetic Factors: Y chromosome microdeletions affecting genes crucial for spermatogenesis
- Environmental Toxins: Heat, radiation, or chemicals disrupting germ cell development
- Infections: Mumps orchitis or sexually transmitted infections damaging seminiferous tubules
Sperm Transport Issues: Even normal sperm production can be ineffective if transport is blocked:
- Vas Deferens Obstruction: Congenital absence or surgical damage
- Epididymal Dysfunction: Impaired sperm maturation and storage
- Ejaculatory Disorders: Retrograde ejaculation or anejaculation
Sperm Function Abnormalities: Sperm may be produced normally but lack fertilization capacity:
- Poor Motility: Defective flagellar structure or energy metabolism
- Abnormal Morphology: Defective head, midpiece, or tail structure
- Acrosome Defects: Inability to penetrate egg zona pellucida
Female Factor Infertility:
Female infertility involves more complex biological systems due to the cyclical nature of female reproduction:
Ovulation Disorders: These account for approximately 25% of female infertility cases:
- Hypothalamic Dysfunction: Disrupted GnRH pulsatility affecting FSH/LH release
- Pituitary Disorders: Hyperprolactinemia or other hormone imbalances
- Ovarian Factors: Polycystic ovary syndrome (PCOS) or premature ovarian failure
- Thyroid Disorders: Affecting overall reproductive hormone balance
Tubal Factor Infertility: Fallopian tube dysfunction prevents normal fertilization:
- Pelvic Inflammatory Disease: Infection-induced scarring and adhesions
- Endometriosis: Inflammatory condition affecting tubal function
- Congenital Abnormalities: Structural defects in tubal development
- Previous Surgery: Scarring from abdominal or pelvic procedures
Uterine and Cervical Factors: These affect implantation and sperm transport:
- Uterine Fibroids: Submucosal fibroids interfering with implantation
- Endometrial Disorders: Inadequate endometrial development
- Cervical Mucus Problems: Hostile cervical environment for sperm
- Congenital Uterine Anomalies: Structural abnormalities affecting pregnancy
In Vitro Fertilization (IVF): Controlled Reproduction in Laboratory
IVF represents the most sophisticated assisted reproductive technology, essentially replicating the early stages of human reproduction in a controlled laboratory environment.
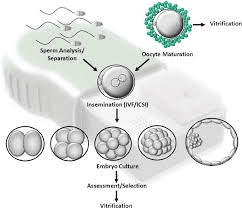
Phase 1: Ovarian Stimulation (Days 1-12)
The biological goal is to stimulate multiple follicle development instead of the single dominant follicle that normally develops each cycle:
Suppression Protocol: GnRH agonists or antagonists suppress the natural LH surge, preventing premature ovulation. The biological mechanism involves:
- Receptor Desensitization: Continuous GnRH agonist exposure causes receptor downregulation
- Pituitary Suppression: Prevents endogenous FSH/LH surges
- Cycle Synchronization: Allows controlled timing of stimulation
Controlled Ovarian Hyperstimulation: Injectable gonadotropins (FSH/LH) stimulate multiple follicle development:
- Follicular Recruitment: Higher FSH levels rescue follicles that would normally undergo atresia
- Synchronized Development: Multiple follicles grow simultaneously
- Monitoring: Serial ultrasounds and hormone levels track follicle development
Phase 2: Oocyte Retrieval (Day 14)
hCG Trigger: Human chorionic gonadotropin injection mimics the natural LH surge, initiating final oocyte maturation:
- Meiosis I Completion: Oocytes complete first meiotic division
- Cumulus Expansion: Surrounding cells prepare for ovulation
- Optimal Timing: Retrieval performed 34-36 hours post-hCG
Transvaginal Aspiration: Oocytes are retrieved through ultrasound-guided needle aspiration:
- Follicular Puncture: Needle enters each mature follicle
- Aspiration: Follicular fluid containing oocyte is collected
- Immediate Assessment: Embryologist identifies and evaluates oocytes
Phase 3: Fertilization (Days 1-2)
Sperm Preparation: Semen sample undergoes processing to select motile, morphologically normal sperm:
- Density Gradient Separation: Removes debris and abnormal sperm
- Washing: Eliminates seminal plasma and concentrates sperm
- Capacitation: Sperm undergo biochemical changes necessary for fertilization
Insemination Methods:
- Conventional IVF: Sperm and eggs are incubated together, allowing natural fertilization
- ICSI (Intracytoplasmic Sperm Injection): Single sperm is directly injected into each egg cytoplasm
Phase 4: Embryo Development (Days 1-6)
Fertilization Assessment: Embryologists monitor for signs of successful fertilization:
- Two Pronuclei: Visible 16-18 hours post-fertilization
- First Cleavage: Cell division begins 24-26 hours post-fertilization
- Continued Development: Daily assessment of embryo quality
Embryo Culture: Embryos develop in specialized culture media that supports:
- Energy Metabolism: Providing appropriate nutrients for each developmental stage
- pH Buffering: Maintaining optimal pH for enzyme function
- Gas Exchange: Controlled oxygen and CO2 concentrations
- Growth Factors: Supporting cellular division and differentiation
Phase 5: Embryo Transfer (Days 3-6)
Embryo Selection: The highest quality embryos are selected based on:
- Morphological Criteria: Cell number, symmetry, and fragmentation
- Developmental Timing: Appropriate progression through cleavage stages
- Blastocyst Formation: Advanced embryos that reach blastocyst stage
Transfer Procedure: Selected embryos are placed in the uterine cavity:
- Catheter Insertion: Soft catheter threaded through cervix into uterus
- Ultrasound Guidance: Ensures optimal placement in uterine fundus
- Minimal Trauma: Gentle technique to avoid endometrial damage
Zygote Intrafallopian Transfer (ZIFT): Combining IVF with Natural Environment
ZIFT represents a hybrid approach that combines laboratory fertilization with placement in the natural environment of the fallopian tube.
Biological Rationale: The fallopian tube provides the optimal environment for early embryonic development:
- Nutrient Gradients: Natural progression of nutrients supporting development
- Growth Factors: Tubal secretions containing embryotrophic factors
- Physical Environment: Appropriate oxygen tension and pH
- Natural Transport: Ciliary action and muscular contractions aid embryo movement
ZIFT Procedure Steps:
- Ovarian Stimulation and Retrieval: Similar to IVF protocol
- Fertilization Verification: Confirmation of fertilization after 18-24 hours
- Laparoscopic Transfer: Fertilized eggs (zygotes) transferred to fallopian tubes
- Natural Development: Embryos develop and travel naturally to uterus
Advantages and Limitations:
Biological Advantages:
- Natural Environment: Early development occurs in optimal tubal environment
- Higher Success Rates: Some studies suggest improved implantation rates
- Natural Selection: Natural barriers may filter out abnormal embryos
Limitations:
- Surgical Requirement: Laparoscopy needed for transfer
- Tubal Patency: Requires at least one functional fallopian tube
- Technical Complexity: More invasive than standard IVF transfer
Gamete Intrafallopian Transfer (GIFT): Fertilization in Natural Environment
GIFT allows fertilization to occur naturally within the fallopian tube while overcoming barriers to natural conception.
Biological Principle: GIFT mimics natural reproduction by placing gametes in their natural meeting place – the ampullary region of the fallopian tube where fertilization normally occurs.
Procedure Overview:
- Ovarian Stimulation: Similar protocol to IVF
- Gamete Retrieval: Both eggs and sperm are collected
- Immediate Transfer: Fresh gametes transferred to fallopian tubes during same procedure
- Natural Fertilization: Fertilization occurs in vivo in tubal environment
Biological Advantages:
- Natural Fertilization Environment: Optimal conditions for sperm-egg interaction
- Natural Selection Pressure: Only viable embryos survive tubal journey
- Hormonal Environment: Natural hormonal milieu supports early development
- Ethical Considerations: Some find natural fertilization more acceptable than IVF
Selection Criteria: GIFT is most appropriate when:
- Unexplained Infertility: Normal gametes but unclear fertilization barriers
- Cervical Factor Infertility: Bypassing cervical mucus hostility
- Mild Male Factor: Sufficient sperm count for natural fertilization
- Functional Tubes: At least one patent, healthy fallopian tube
Success Rates and Factors: GIFT success depends on:
- Age: Maternal age significantly affects success rates
- Tubal Health: Optimal tubal environment essential
- Gamete Quality: Both sperm and egg quality influence outcomes
- Number of Embryos: Multiple gamete transfers increase pregnancy rates
Biological Factors Affecting ART Success
Maternal Age Effects: Advanced maternal age affects multiple biological processes:
- Oocyte Quality: Increased chromosomal abnormalities with age
- Mitochondrial Function: Reduced energy production in aging eggs
- Endometrial Receptivity: Decreased implantation potential
- Hormone Production: Altered reproductive hormone patterns
Embryo Quality Assessment: Modern ART uses sophisticated methods to evaluate embryo viability:
- Time-lapse Imaging: Continuous monitoring of embryo development
- Metabolic Profiling: Analyzing embryo energy metabolism
- Genetic Screening: Preimplantation genetic testing for chromosomal abnormalities
- Morphokinetic Analysis: Timing of developmental milestones
Endometrial Receptivity: The “implantation window” represents a brief period when the endometrium is receptive to embryo implantation:
- Molecular Markers: Expression of specific genes and proteins
- Morphological Changes: Pinopode formation and glandular secretions
- Hormonal Preparation: Optimal estrogen and progesterone exposure
- Immune Modulation: Local immunosuppression allowing embryo acceptance
Real-World Biology Connection: The first IVF baby, Louise Brown, was born in 1978. Since then, over 8 million babies have been born worldwide through ART, demonstrating how understanding reproductive biology has revolutionized treatment of infertility.
7: Advanced Applications and Current Research in Reproductive Health
Emerging Technologies and Future Directions
The field of reproductive health continues to evolve rapidly, with new technologies building on fundamental biological principles to address previously untreatable conditions.
Mitochondrial Replacement Therapy: This technique addresses mitochondrial DNA disorders by replacing defective mitochondria:
- Three-Parent IVF: Combines nuclear DNA from two parents with healthy mitochondria from a donor
- Biological Rationale: Mitochondrial disorders affect cellular energy production
- Ethical Considerations: Heritable genetic modifications raise complex questions
Artificial Gametes: Research into creating sperm and eggs from stem cells could revolutionize fertility treatment:
- Induced Pluripotent Stem Cells: Reprogramming adult cells to embryonic-like state
- Gametogenesis in Culture: Directing stem cell differentiation into functional gametes
- Clinical Applications: Potential treatment for patients with no viable gametes
Uterine Transplantation: Recent successes in uterine transplants offer hope for women with uterine factor infertility:
- Immunological Challenges: Preventing rejection while allowing pregnancy
- Surgical Complexity: Vascular connections and organ positioning
- Pregnancy Management: Monitoring fetal development in transplanted uterus
Personalized Reproductive Medicine
Genetic Screening Advances: Comprehensive genetic analysis is becoming standard in reproductive medicine:
- Whole Genome Sequencing: Complete genetic analysis of embryos
- Polygenic Risk Scores: Assessing complex trait risks
- Pharmacogenomics: Tailoring medications based on genetic profiles
Biomarker Development: Research focuses on identifying markers that predict reproductive outcomes:
- Ovarian Reserve Testing: Multiple markers assess remaining egg quantity
- Implantation Predictors: Molecular signatures indicating optimal transfer timing
- Male Fertility Assessment: Advanced sperm function tests beyond basic parameters
Global Health Perspectives
Reproductive Health Disparities: Understanding biological factors in different populations:
- Genetic Diversity: Population-specific genetic variants affecting fertility
- Environmental Influences: Geographic and socioeconomic factors on reproductive health
- Cultural Considerations: Integrating traditional practices with modern medicine
8: Practice Problems and Application Exercises
Multiple Choice Questions with Detailed Solutions
Question 1: Which of the following best explains why combined oral contraceptives are more effective than progestin-only pills?
A) Combined pills contain higher hormone concentrations
B) Combined pills suppress ovulation more completely through dual hormone action
C) Progestin-only pills have more side effects
D) Combined pills are taken more frequently
Solution: The correct answer is B. Combined oral contraceptives contain both synthetic estrogen and progestin, which work together to suppress the hypothalamic-pituitary-ovarian axis more effectively than progestin alone. The estrogen component enhances the suppression of FSH, preventing follicular development, while progestin suppresses LH, preventing ovulation. This dual mechanism provides more complete ovarian suppression compared to progestin-only pills, which primarily work by altering cervical mucus and endometrial lining rather than completely preventing ovulation.
Question 2: A couple undergoes IVF treatment, and 8 oocytes are retrieved. After fertilization assessment, 6 show normal fertilization with two pronuclei. On day 3, embryo quality assessment reveals: 2 embryos with 8 cells and minimal fragmentation, 2 embryos with 6 cells and moderate fragmentation, and 2 embryos with irregular cell division. Which embryos should be selected for transfer?
A) All 6 fertilized embryos
B) Only the 8-cell embryos with minimal fragmentation
C) The 8-cell and 6-cell embryos combined
D) Only the embryos with irregular division
Solution: The correct answer is B. Embryo selection is based on developmental timing and morphological quality. On day 3 post-fertilization, optimal embryos should have 7-9 cells with minimal fragmentation (<10%). The 8-cell embryos with minimal fragmentation represent the highest quality with the best implantation potential. The 6-cell embryos with moderate fragmentation have lower quality due to slower development and increased fragmentation, while embryos with irregular cell division have poor developmental potential and higher chromosomal abnormality risk.
Question 3: A 35-year-old woman undergoes amniocentesis at 16 weeks gestation. The karyotype analysis reveals 47,XX,+21. What does this result indicate?
A) Normal female karyotype
B) Turner syndrome
C) Down syndrome
D) Klinefelter syndrome
Solution: The correct answer is C. The karyotype 47,XX,+21 indicates trisomy 21 (Down syndrome). The notation means there are 47 total chromosomes instead of the normal 46, with an extra copy of chromosome 21. This condition results from nondisjunction during meiosis, most commonly in maternal meiosis I, and the risk increases with maternal age. The XX indicates female sex chromosomes, so this would be a female fetus with Down syndrome.
Case Study Analysis Problems
Case Study 1: Contraceptive Method Selection
Sarah is a 28-year-old woman who wants effective contraception but has a history of blood clots and smoking. She’s considering various options and seeks advice about the most appropriate method.
Biological Analysis Required:
- Evaluate thrombotic risk factors
- Consider hormone-related contraindications
- Assess method effectiveness and safety profile
- Recommend evidence-based options
Complete Solution:
Sarah’s history of blood clots and smoking creates significant contraindications for estrogen-containing contraceptives. Combined oral contraceptives, patches, and rings all contain estrogen, which increases thrombotic risk through effects on coagulation factors. Smoking further increases this risk by promoting endothelial dysfunction and platelet aggregation.
Appropriate options include:
- Progestin-only methods: Pills, injections, or implants don’t increase clot risk
- Copper IUD: Highly effective non-hormonal option
- Barrier methods: Condoms or diaphragms with spermicide
- Sterilization: If she desires permanent contraception
The copper IUD would be optimal, providing >99% effectiveness for 10 years without hormonal risks. Progestin-only options are also suitable but may have other side effects to consider.
Case Study 2: Infertility Investigation
Mark (32) and Lisa (29) have been trying to conceive for 18 months without success. Lisa has regular 28-day cycles, and Mark’s semen analysis shows: volume 3.2ml, concentration 18 million/ml, motility 35%, normal morphology 3%.
Biological Analysis Required:
- Interpret semen parameters against normal values
- Identify potential fertility factors
- Suggest appropriate investigations
- Recommend treatment options
Complete Solution:
Semen Analysis Interpretation:
- Volume: Normal (>1.5ml)
- Concentration: Below normal (normal >15 million/ml, but borderline)
- Motility: Below normal (normal >40% progressive motility)
- Morphology: Below normal (normal >4% strict criteria)
Mark shows oligoasthenoteratozoospermia (low count, poor motility, abnormal morphology), indicating male factor infertility. Lisa’s regular cycles suggest normal ovulation, but further evaluation needed.
Additional Investigations:
- Hormone testing (FSH, LH, testosterone) for Mark
- Tubal assessment (HSG or laparoscopy) for Lisa
- Ovulation confirmation (progesterone levels, ultrasound)
- Genetic testing if severe male factor
Treatment Options:
- Lifestyle modifications (diet, exercise, antioxidants)
- IUI with sperm preparation if mild male factor
- IVF with ICSI if severe male factor
- Address any female factors identified
Experimental Design Questions
Question: Design an experiment to test the effectiveness of a new spermicidal agent compared to nonoxynol-9.
Complete Experimental Design:
Hypothesis: The new spermicidal agent will demonstrate superior contraceptive effectiveness compared to nonoxynol-9 with reduced side effects.
Study Design: Randomized, double-blind, controlled clinical trial
Participants:
- 1000 sexually active women aged 18-35
- Regular menstrual cycles
- No contraindications to spermicide use
- Informed consent obtained
Randomization:
- Group A (n=500): New spermicidal agent
- Group B (n=500): Nonoxynol-9 control
Primary Endpoints:
- Pearl Index (pregnancies per 100 woman-years)
- Time to pregnancy occurrence
- Contraceptive failure rate
Secondary Endpoints:
- Vaginal irritation incidence
- UTI frequency
- STI transmission rates
- User satisfaction scores
Laboratory Assessments:
- In vitro sperm immobilization assays
- Cytotoxicity testing on vaginal epithelial cells
- pH effects on vaginal environment
- Residual contraceptive activity over time
Statistical Analysis:
- Chi-square tests for categorical outcomes
- Kaplan-Meier survival analysis for time-to-pregnancy
- Logistic regression adjusting for confounders
- Power analysis: 80% power to detect 20% difference
Ethical Considerations:
- IRB approval required
- Informed consent process
- Safety monitoring board
- Pregnancy counseling and support
Data Analysis and Interpretation Problems
Problem: Analyze the following IVF success rate data and explain the biological factors contributing to the observed patterns:
| Age Group | Cycles Started | Live Birth Rate | Miscarriage Rate |
|---|---|---|---|
| <35 years | 1000 | 45% | 15% |
| 35-37 years | 800 | 35% | 20% |
| 38-40 years | 600 | 25% | 30% |
| 41-42 years | 400 | 15% | 40% |
| >42 years | 200 | 8% | 50% |
Complete Analysis:
Observed Patterns:
- Declining Success Rates: Live birth rates decrease significantly with increasing maternal age
- Increasing Miscarriage Rates: Pregnancy loss rates double from youngest to oldest groups
- Steeper Decline After 35: Most dramatic changes occur after age 35
Biological Explanations:
Oocyte Quality Decline:
- Chromosomal Abnormalities: Increased aneuploidy with aging oocytes due to deteriorating cohesin proteins holding sister chromatids together
- Mitochondrial Dysfunction: Reduced energy production affects fertilization and early embryonic development
- Cumulus Cell Quality: Decreased communication between oocyte and surrounding cells affects maturation
Hormonal Changes:
- Reduced Ovarian Reserve: Declining AMH and rising FSH levels indicate fewer remaining follicles
- Altered Hormone Dynamics: Changed FSH sensitivity affects follicular development
- Luteal Phase Defects: Inadequate progesterone production affects implantation
Endometrial Factors:
- Decreased Receptivity: Aging endometrium shows reduced implantation markers
- Vascular Changes: Altered uterine blood flow affects embryo support
- Immune Dysfunction: Changes in local immune environment affect implantation success
Clinical Implications:
- Earlier fertility treatment initiation for women >35
- Consideration of donor oocytes for women >40
- Preimplantation genetic screening to reduce miscarriage risk
- Individualized protocols based on ovarian reserve markers
Exam Preparation Strategies and Common Mistakes
High-Yield Topics for CBSE Board Exams
Frequently Tested Concepts:
- Contraceptive Method Mechanisms: Understanding how different methods prevent pregnancy at cellular and physiological levels
- STD Prevention and Treatment: Pathogen-specific prevention strategies and biological rationale
- Hormonal Regulation: Role of reproductive hormones in natural cycles and artificial manipulation
- ART Procedures: Step-by-step understanding of IVF, ZIFT, and GIFT processes
- Genetic Screening: Applications and limitations of prenatal diagnosis
Common Student Errors and Prevention
Error 1: Confusing Contraceptive Mechanisms
Common Mistake: Students often confuse how barrier methods work versus hormonal methods.
Prevention Strategy: Create a systematic classification:
- Physical barriers: Prevent sperm-egg contact
- Chemical barriers: Kill or immobilize sperm
- Hormonal methods: Suppress ovulation and alter reproductive tract
- Surgical methods: Permanently block gamete transport
Error 2: Misunderstanding ART Success Factors
Common Mistake: Assuming all ART methods have similar success rates and indications.
Prevention Strategy:
- Study specific indications for each procedure
- Understand why success rates vary by method and patient factors
- Connect biological mechanisms to clinical outcomes
Error 3: Inadequate STD Knowledge
Common Mistake: Memorizing disease names without understanding transmission mechanisms.
Prevention Strategy:
- Group STDs by pathogen type (bacterial, viral, parasitic)
- Study transmission routes and prevention methods
- Connect pathogen characteristics to clinical presentations
Effective Study Techniques
Memory Techniques:
Mnemonics for Contraceptive Methods:
- BIHS: Barrier, Intrauterine, Hormonal, Surgical
- Natural methods: Calendar, Cervical, Coitus (withdrawal)
Hormone Sequence Memory Aid:
- GnRH → FSH/LH → Estrogen/Progesterone → Target Effects
Answer Writing Strategies
Structured Answer Format:
- Define key terms in the first sentence
- Explain biological mechanisms with specific details
- Provide relevant examples or applications
- Connect to broader concepts when appropriate
- Conclude with significance or implications
Example Answer Structure for “Explain IVF procedure”:
Introduction: Define IVF as assisted reproductive technology involving fertilization outside the body
Main Content:
- Ovarian stimulation process and biological rationale
- Oocyte retrieval technique and timing
- Fertilization methods and assessment
- Embryo development and selection criteria
- Transfer procedure and success factors
Conclusion: Significance for treating infertility and success rate factors
Conclusion and Future Directions in Reproductive Health
As you complete your study of reproductive health, it’s important to recognize that this field represents one of the most dynamic areas in modern biology and medicine. The concepts you’ve mastered – from basic contraceptive mechanisms to advanced assisted reproductive technologies – form the foundation for understanding how biological knowledge translates into practical solutions for human health challenges.
The journey through this chapter has taken you from fundamental reproductive biology to cutting-edge medical technologies. You’ve explored how understanding hormonal regulation led to the development of contraceptive pills, how knowledge of fertilization biology enabled IVF technology, and how advances in genetics revolutionized prenatal diagnosis. These connections between basic biology and clinical applications exemplify how scientific understanding drives medical progress.
Key Concepts to Remember:
Your mastery of reproductive health concepts extends far beyond exam preparation. The biological principles you’ve learned – hormone regulation, cellular processes, genetic mechanisms, and physiological systems – apply to numerous other areas of biology and medicine. Understanding reproductive health also provides insights into evolution, development, genetics, and biotechnology.
Real-World Applications:
The reproductive health field continues evolving rapidly. Current research focuses on personalized medicine approaches, using genetic information to optimize fertility treatments. Scientists are developing better contraceptive methods with fewer side effects, improving assisted reproductive technologies, and advancing prenatal diagnosis capabilities. Your understanding of fundamental concepts prepares you to appreciate and contribute to these advances.
Career Connections:
Knowledge of reproductive health opens pathways to diverse careers in medicine, research, biotechnology, and public health. Whether you pursue gynecology, reproductive endocrinology, genetic counseling, biotechnology research, or public health policy, the concepts you’ve learned provide essential background knowledge.
Continuing Your Learning:
As you prepare for your CBSE examination and beyond, remember that reproductive health represents a perfect example of applied biology. The success of your exam preparation depends on connecting theoretical knowledge with practical applications, understanding mechanisms rather than memorizing facts, and appreciating the broader significance of reproductive health in human society.
The field’s rapid evolution means that lifelong learning is essential for anyone working in reproductive health. Stay curious about new developments, connect with current research, and remember that today’s cutting-edge technologies often build on the fundamental biological principles you’re mastering now.
Your journey through reproductive health concepts demonstrates the power of biological knowledge to address fundamental human needs. From family planning to treating infertility, from preventing disease to ensuring healthy pregnancies, reproductive health touches every aspect of human reproduction and development.
Final Exam Success Tips:
Focus on understanding biological mechanisms rather than memorizing isolated facts. Practice explaining concepts in your own words, work through diverse problem types, and connect reproductive health concepts to other areas of biology you’ve studied. Remember that CBSE exams reward comprehensive understanding and the ability to apply knowledge to new situations.
The time you’ve invested in mastering reproductive health concepts will serve you well, not just in examinations, but in understanding one of biology’s most important and fascinating fields. Whether you pursue advanced studies in biology, enter medical fields, or simply apply this knowledge as an informed citizen, you’ve built a solid foundation for lifelong learning and contribution to human health and well-being.
References and Further Reading:
- NCERT Class 12 Biology Textbook
- Human Reproductive Biology – Jones & Lopez
- Principles of Assisted Reproductive Technology – Gardner & Weissman
- WHO Guidelines on Reproductive Health
- Current Research in Reproductive Medicine Journals
Practice Resources:
- CBSE Previous Year Question Papers
- NCERT Exemplar Problems
- All India Medical Entrance Exam Questions
- Interactive Biology Simulations
- Medical Case Study Collections
This comprehensive study guide provides you with the knowledge, understanding, and exam strategies needed to excel in CBSE Class 12 Biology Chapter 3: Reproductive Health. Use it as your primary resource for mastering this crucial topic and achieving academic success.
Recommended –

1 thought on “Class 12 Biology Chapter 3: Reproductive Health – Complete Notes with NCERT Solutions”